Settling in for a flight is never the same once you’ve taken the Hippocratic Oath. In the back of your mind is always the fear of hearing the dreaded message asking if there is a doctor on board.
Settling in for a flight is never the same once you’ve taken the Hippocratic Oath. In the back of your mind is always the fear of hearing the dreaded message asking if there is a doctor on board.
But how likely is it that you’ll need to perform an in-flight trachestomy with only a coat hanger? And what assistance can you expect at 30,000ft? JuniorDr’s Ben Chandler finds out.
Cramped in a cabin with up to 850 other anxious passengers isn’t the best place to practice medicine. Add in the effects of engine noise, cabin pressure and a limited supply of unfamiliar equipment and it can become your worst nightmare.
Unfortunately with an ageing population and greater passenger numbers your chance of facing a medical emergency whilst jetting off on your summer holiday is on the rise. With between 1 and 10 incidents per 40,000 passengers(1) it’s a scenario that many doctors will face at some point in their careers.
In-flight emergencies
There have been numerous documented medical incidents in the air but perhaps the most famous occurred in 1995 between Hong-Kong and London. A female patient developed chest pain and dyspnoea shortly after take off and was seen by two doctors onboard.
Having diagnosed a tension pneumothorax they proceeded to insert a chest drain using brandy as disinfectant, a coat hanger as a trochar and bottle of Evian water as an underwater seal. The flight continued and the patient was eventually seen in a hospital in the UK where she made an uncomplicated recovery(2).
But before you start revising chest drain insertion it is useful to know that this is one of the more rare emergencies you are likely to face. Most cases are due to exacerbation of pre-existing medical conditions, either from the aircraft effects such as cabin pressure or the stress of flying,
or medication problems such as accidentally packing important medication in the hold.
Syncope is by far the commonest, making up around 50% of cases. Gastro-intestinal upset and generalised pains are the next most frequent – possibly related to dehydration, alcohol consumption and disrupted sleep. Fortunately many emergencies will be dealt with by airline staff without the assistance of onboard doctors.
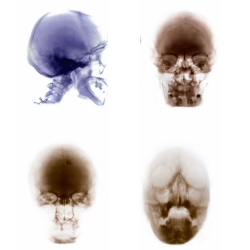
Cabin pressure
Travelling by commercial airliner exerts various effects on the body that can precipitate medical difficulties. The most immediate is the lower ambient pressure which causes a drop in oxygen saturations to around 90% even in healthy passengers.
Airline cabin pressures are usually equivalent to 2000-2400 metres altitude, and passengers with underlying heart or chest disease may require additional oxygen to counter hypoxia. Most people experience the expansion of gas in air filled cavities on take-off manifesting as pain in the ears or sinuses but it also has the potential to convert a simple pneumothorax into a tension pneumothorax.
Relative humidity is low in the cabin, causing dehydration, worsened by alcohol. The risks of deep vein thrombosis from limited mobility and dehydration are well recognised as the infamous ‘economy class syndrome’.
Airline defibrillators
Over recent years the amount and type of emergency equipment carried on aeroplanes has been reviewed with many airlines now carrying automated external defibrillators (AEDs).
One person who has benefited from this is MP Paul Keetch. In 2007 Mr Keetch suffered a cardiac arrest whilst on a Virgin Atlantic flight from Heathrow to New York. He was successfully defibrillated and returned to Heathrow for hospital treatment.
In a recently published study one major US airline reported 200 uses of AEDs over a 2 year period, including 13 defibrillations. They found a 40% survival rate for VF or pulseless VT arrests – remarkable when you consider the difficult cabin environment.(3)
Emergency Landings
Many of these medical scenarios can be dealt with in the air avoiding unnecessary emergency landings, however in around 1-2% of cases an emergency diversion is necessary. This is potentially a very expensive decision with the overall cost as much as £125,000 to divert a plane.(5)
If other passengers are left stranded for any reason, then hotel bills and other expenses can increase dramatically. In 1996 a passenger on a Virgin Atlantic flight had a suspected heart attack, and the flight diverted to a small airport in Eastern Canada.
However during the landing one of the aeroplanes’ engines was damaged. Nearly 400 passengers (including pop star Gary Barlow) were left stranded for 15 hours at the local curling rink while other aeroplanes were sent to pick them up.(6)
Support from the ground
If called upon to help you are unlikely to be totally alone. On any flight there is approximately a 60-85% chance of there being a doctor as a passenger onboard7 and most flight attendants are trained to deal with common medical emergencies.
Many airlines also have access to MedLink, the largest medical support service with experienced emergency doctors on hand to offer advice.
“In this scenario the medical volunteer assumes a position of being the eyes and hands, helping in assessing and administering medication,” says Dr Paulo Alves, the Vice-President of MedAire, who run the service.
“The MedLink Physician will have the experience and emotional detachment to help with situation onboard, and help the captain to make the best decision about landing or not.”
Medlink is run from Pheonix USA, and is staffed by emergency doctors with training in aviation medicine. They deal with nearly 100 cases per day.
As well as supplying medical knowledge they also have access to a database of medical resources and details of runways around the globe, so they can advise on the most suitable diversion should it be necessary.
Interest is now growing in telemedical devices which will allow vital signs, ECG and other data to be transmitted to staff on the ground. This technology has already been taken up by several airlines.
Good Samaritan Acts
Many doctors have concerns that they could potentially be the subject of medico-legal action arising from their decisions during an aeroplane medical emergency. The legal position is complicated as it is different in different countries.
Despite this the GMC and BMA stance is that doctors should assist if required. Indemnity against prosecution may be offered by the airline, but this may depend on whether you were asked to help.
Both the MPS and MDU cover their members for actions taken while on a plane. The MPS suggest that before getting involved doctors should clearly state their competencies and skills, as well as other factors that may affect their performance, such as alcohol.(8)
So if you ever hear those dreaded words over the airline tannoy, keep in mind to do simple interventions, recognise your own limits, and in most cases there should be help of some kind available.
References
1. Surgical ad Medical emergencies onboard European aircraft. Sand M, Falk-Georges B,
Sand D, Mann B. Critical Care, 2009. 13:1 2. Managing in flight emergencies. Wallace W.
BMJ, 1995;311:374-375
3. Use of Automated External Defibrillators by a U.S. Airline. Page R, Joglar JA, Kowal R,
Zagrodzky J, et al. NEJM, 2000; 343:1210-1216
4. Federal Aviation Authority Advisory Circular, 2006. www.rgl.faa.gov
5. How much does an airline diversion cost. Martin G. www.gadling.com
6. Unexpected Arctic stop for Brits, Yanks. Van Rassel J. Nunatsiaq News 1996.
7. Health Issues of air travel. DeHart R. Annual Review of Public Health, 2003; 24: 133-151
8. Flying doctors: is protection plain. Williams S. Casebook 2008; 16: 8-11